The timing of implant placement affects both treatment planning and long-term outcomes. Immediate dental implants involve placing an implant on the same day a tooth is removed. This approach is only considered when bone quality, gum health, and overall anatomy support safe and predictable placement.
Immediate implants are not a quicker or universal solution. They require a detailed clinical evaluation. Dentists assess the extraction site, surrounding tissues, and the patient’s general oral health before deciding whether the procedure is suitable.
This guide explains what immediate placement involves and how it differs from the traditional delayed method. It also outlines the factors that influence eligibility. The aim is to offer clear and patient-friendly information for people exploring implant options.
Note: This article provides general information. It cannot replace a full clinical assessment, radiographic imaging, or personalised advice from a qualified dentist.
What Are Immediate Dental Implants?
Immediate dental implants are implants placed directly into the socket right after a tooth is removed. Unlike the delayed method—where the site heals for weeks or months—the immediate approach uses the existing socket as the placement area. This is only possible when the bone and surrounding tissues are healthy enough to support stable positioning.
The most important requirement is primary stability. This means the implant must lock firmly into the bone at the moment of placement. Stability depends on:
Bone density
Shape of the socket
Condition of the surrounding gum and bone
When these factors are favourable, immediate placement may help maintain the natural shape of the bone and gums. This can support a more conservative approach to site preservation.
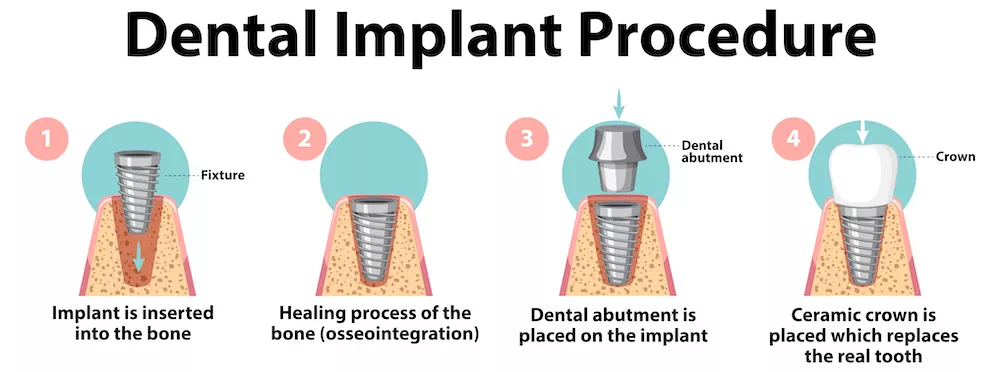
It is important to understand that “immediate” does not mean “faster healing.” The biological process—especially osseointegration, where bone bonds to the implant—follows its usual timeline. Temporary teeth may sometimes be placed for appearance only, but they are not used for normal chewing unless the dentist confirms that the implant can safely handle it.
Immediate implants are one treatment option, not a universal solution. Suitability depends on a full evaluation that includes:
Clinical examination
Radiographic imaging
Bone and gum assessment
Oral hygiene review
Infection risk analysis
Only after this evaluation can a dentist decide whether immediate placement is appropriate or whether a delayed approach is safer.
Immediate vs. Delayed Implant Placement: Understanding the Differences
Choosing between immediate and delayed implant placement depends on anatomy, healing needs, and long-term predictability. Both methods aim to restore function and support oral health, but they differ in timing and treatment steps. This section provides general information and does not replace personalised clinical advice.
Immediate Dental Implants: A Timing-Based Approach
In immediate placement, the implant is inserted during the same appointment as the extraction. The existing socket guides positioning, and the natural contours of the tissues may be easier to preserve.
Key characteristics include:
Implant placed at the extraction visit
Requires intact and healthy socket walls
Primary stability must be achievable at surgery
Healing still follows the standard osseointegration timeline
Immediate placement does not speed up healing. It only changes when the implant is placed, not how bone integration occurs.
Delayed Implant Placement: A Staged, Conventional Method
In delayed placement, the dentist waits weeks or months after extraction. This allows the bone and gum tissue to stabilise before the implant is inserted.
It may be preferred when:
Bone quality is low
There is active or recent infection
Socket walls are damaged or missing
Grafting or regeneration is needed
Soft tissue requires healing time
This approach provides a controlled environment and is suitable for many clinical situations.
Comparing the Two Approaches
| Consideration | Immediate Placement | Delayed Placement |
|---|---|---|
| Timing | Same session as extraction | Weeks–months after extraction |
| Primary stability requirement | High | Achieved after healing |
| Socket preservation | May help maintain natural contours | May require grafting |
| Suitability | Case-specific, ideal conditions needed | Broadly applicable |
| Healing | Standard osseointegration | Standard osseointegration |
Both methods can be successful when applied to the right case.
Why the Distinction Matters
Patients often associate “faster” with “better,” but implant success depends on:
Anatomical suitability
Healing needs
Long-term stability
For some cases, immediate implants may be considered. For others, a staged approach provides a safer and more predictable outcome.
Immediate vs. Delayed Implant Placement: Understanding the Differences
Choosing between immediate and delayed implant placement is a clinical decision based on anatomy, healing dynamics, and long-term predictability. Both approaches aim to restore function and support oral health, but they differ in timing, biological processes, and the steps involved in treatment planning. The information below is intended for educational purposes and should not be interpreted as a personalised treatment pathway. Only a comprehensive clinical evaluation can determine which method is appropriate.
Immediate Dental Implants: A Timing-Based Approach
With immediate dental implants, the implant is placed directly after extraction. The advantage of this timing is that the existing socket can help guide placement, and the natural contours of the bone and soft tissue may be better preserved.
Key characteristics include:
Placement during the same visit as the tooth extraction
Requires intact and healthy socket walls
Primary stability must be achievable at the time of surgery
Healing still follows a standard osseointegration period, regardless of timing
Immediate placement does not accelerate biological healing. It simply changes when the implant is inserted, not how bone integration occurs.
Delayed Implant Placement: A Staged, Conventional Method
Delayed placement is the traditional approach, where clinicians wait weeks or months after extraction before inserting the implant. This allows the site to heal fully and provides the clinician with a predictable, stabilised foundation.
It may be preferred when:
Bone quality is insufficient for primary stability
There is active or recent infection
The socket walls are damaged or missing
Additional grafting or regeneration is needed
Soft tissue requires time to stabilise
The delayed approach can offer a controlled environment for implants, especially when the initial extraction site presents uncertainties.
Comparing the Two Approaches
| Consideration | Immediate Placement | Delayed Placement |
|---|---|---|
| Timing | Same session as extraction | Weeks–months after extraction |
| Primary stability requirement | High | Achieved after healing |
| Socket preservation | May help maintain natural contours | May require grafting depending on healing |
| Suitability | Case-specific, requires ideal conditions | Broadly applicable in many clinical scenarios |
| Healing | Standard osseointegration timeline | Standard osseointegration timeline |
Both methods can offer successful outcomes when applied in appropriate clinical situations. The choice depends on the health of the extraction site, diagnostic imaging, and the overall treatment plan.
Why the Distinction Matters
Patients often assume “faster” means “better,” but in dentistry, timing is only one aspect of success. The decision must balance anatomical suitability, long-term stability, and biological healing. For some cases, immediate dental implants may be considered; for others, the staged approach provides safer predictability.

How Immediate Dental Implants Are Planned and Placed
Immediate dental implants require detailed planning and careful surgical execution. Because the implant is placed on the same day as the extraction, the dentist must confirm that the site provides safe and predictable stability. The outline below is for educational purposes only and does not replace personalised clinical advice.
Comprehensive Diagnostic Evaluation
Planning begins with a full clinical assessment and detailed imaging.
Clinical Assessment
The dentist examines the tooth that needs removal, checks gum health, and looks for signs of infection or inflammation. Any active infection may reduce the chances of immediate placement.
Radiographic Imaging (CBCT)
A CBCT scan helps assess:
Bone density
Socket shape
Nerve and sinus proximity
Hidden pathology
These details guide decisions about implant size, angle, and position.
Systemic and Oral Health Review
Factors such as smoking, diabetes, and oral hygiene habits influence healing and may affect the timing of implant placement.
Tooth Extraction and Site Preparation
If the case appears suitable, the next step is an atraumatic extraction. This technique protects the surrounding bone and gum tissue, especially the buccal (outer) plate.
Site preparation may include:
Removing residual infection
Inspecting socket walls
Aligning the implant path with anatomical structures
Preserving socket integrity supports stability and long-term outcomes.
Achieving Primary Stability
Primary stability is essential in immediate placement. The implant must anchor firmly into the deeper bone.
Stability depends on:
Bone density
Implant length and diameter
Insertion angle
Condition of the bone plates
If primary stability cannot be achieved, a delayed approach is usually safer.
Bone Grafting When Needed
Some cases require grafting to fill the gap between the implant and socket wall, known as the “jumping gap.” Grafting supports long-term bone preservation. The need for grafting depends on socket size and bone structure.
Soft-Tissue Management
Healthy soft tissue supports long-term implant success. Dentists may use:
Collagen matrices
Connective tissue grafts
Temporary healing abutments
These techniques help maintain gum contour and support stable healing.
Temporary Restorations (If Appropriate)
Temporary restorations are sometimes placed for appearance only. They are shaped so they do not apply pressure to the implant. They are not used for chewing until the dentist confirms that stability and healing allow it.
Post-Placement Monitoring
After placement, the implant enters the healing phase. Follow-up visits allow the dentist to check:
Soft-tissue response
Implant stability
Radiographic signs of integration
Oral hygiene practices
The final restoration is only placed once the implant has integrated successfully.
Benefits of Immediate Dental Implants (Explained with Clinical Balance)
When used in suitable cases, immediate dental implants may offer several potential advantages. These benefits are not guaranteed. Each outcome depends on anatomy, bone quality, gum health, and clinical planning. The points below are for general information only.
1. Preservation of Natural Bone Architecture
After an extraction, the surrounding bone can begin to shrink. Placing an implant immediately may help:
Maintain bone height and width
Support socket stability
Reduce early bone remodelling
This depends on the condition of the socket walls and bone density.
2. Support for Soft-Tissue Contour
Gum shape is important for aesthetic outcomes. Immediate placement may help preserve natural soft-tissue contours, especially when:
The facial bone is intact
Keratinised tissue is adequate
The site has healthy soft tissue
Predictability varies between patients, so clinicians assess this carefully.
3. Reduced Number of Surgical Sessions
Extraction and implant placement occur in the same appointment. This may reduce the number of early surgical visits.
However:
Healing time does not change
Osseointegration still requires several months
The benefit is related to treatment flow, not faster biological healing.
4. Earlier Aesthetic Provisionalisation (When Suitable)
In select cases, dentists may provide a temporary, non-functional restoration. This can help with appearance and soft-tissue shaping.
The temporary is used only when:
Primary stability is confirmed
Bite forces are manageable
The soft tissue is suitable
It is not used for normal chewing.
5. A More Streamlined Treatment Experience
Completing extraction and placement in one visit may make the early stage of treatment feel more structured.
Follow-up visits and long-term reviews remain essential.
Limitations and Considerations of Immediate Dental Implants
Immediate dental implants are not suitable for every case. Understanding their limitations helps set realistic expectations. The points below offer general information and do not replace a personalised clinical assessment.
1. Not All Extraction Sites Allow Immediate Placement
Immediate implants rely on healthy, stable socket walls. Challenges include:
Thin or damaged buccal bone
Large defects around the extraction site
Irregular socket shape
When stability cannot be achieved, a delayed approach is safer.
2. Active Infection May Delay Treatment
Severe infection or widespread inflammation can reduce predictability. Even if some local infections can be managed during extraction, significant infection usually requires healing before implant placement.
3. Primary Stability Is Not Always Possible
Immediate placement needs strong mechanical anchorage. Stability depends on:
Bone density
Socket width
Implant dimensions
Anatomical limits
If sufficient stability cannot be achieved, dentists avoid immediate placement.
4. Soft-Tissue Conditions May Limit Predictability
Healthy gum tissue is essential for long-term success. Immediate placement may be less reliable when:
Keratinised tissue is limited
Gum recession is likely
Soft tissue is thin or fragile
Periodontal disease is present
In such cases, waiting may provide more stable outcomes.
5. Additional Procedures May Be Needed
Immediate placement does not remove the need for grafting. Dentists may recommend:
Bone grafts
Collagen membranes
Connective tissue grafts
Socket preservation techniques
These procedures support long-term stability.
6. Systemic and Lifestyle Factors Affect Healing
Certain factors influence bone and tissue healing, such as:
Uncontrolled diabetes
Smoking
Conditions affecting bone metabolism
Poor oral hygiene
These factors do not always prevent immediate placement, but they may make healing less predictable.
7. Expectations Must Match Biological Realities
Immediate implants do not speed up osseointegration. The implant still needs time to bond with the bone.
Functional chewing is not allowed until the dentist confirms full integration.
Healing and Osseointegration After Immediate Dental Implants
Healing after immediate dental implants follows the same biological process as any implant treatment. Although the implant is placed at the time of extraction, the integration timeline does not speed up. Bone still needs time to bond with the implant surface. The points below explain the general stages of healing.
1. Early Healing Phase (First Few Weeks)
In the first weeks, the extraction socket begins to repair itself.
During this stage:
Soft tissues start closing around the implant
Early bone healing begins
Mild swelling or discomfort may appear
The implant must stay free from chewing forces
Any micro-movement can interfere with stable integration.
2. Bone Integration Phase (Several Weeks to Months)
Osseointegration continues over the following months.
Key changes include:
Bone attaching to the implant surface
Stability shifting from mechanical to biological
Progress checked through radiographic reviews
The timeline is similar to delayed placement, even though the implant was placed earlier.
3. Role of Soft Tissue in Healing
Healthy soft tissue supports long-term stability.
It helps:
Protect the implant–gum interface
Maintain hygiene around the implant
Shape the final aesthetic result
If a temporary restoration is placed, it is adjusted to avoid pressure on the implant.
4. Importance of Follow-Up Appointments
Regular follow-up visits allow the dentist to check:
Gum healing
Signs of inflammation
Implant stability
Oral hygiene habits
These reviews help identify early problems that could affect the outcome.
5. Final Restoration After Confirmed Stability
The final crown is placed only when the dentist confirms that the implant is fully integrated.
The decision is based on:
Clinical stability tests
Imaging results
Soft-tissue health
Overall oral hygiene
Immediate placement does not change these requirements.
Why Immediate Dental Implants Are Not Suitable for Everyone
Immediate dental implants are not appropriate for every situation. Their success depends on bone quality, gum health, infection status, and overall medical condition. A full clinical examination and radiographic imaging are required to confirm suitability. The points below provide general information.
1. Anatomical Requirements Must Be Met
Immediate placement depends on adequate bone volume and density. It may not be suitable when:
Buccal or facial bone walls are thin
Large bone defects are present
The socket has an irregular shape
The implant is too close to the sinus or nerves
In such cases, delayed placement may offer more predictable results.
2. Infection Can Reduce Predictability
Active infection in the extraction site can affect early healing.
Severe infection often requires treatment and healing before implant placement.
3. Gum Health and Soft-Tissue Volume Matter
Healthy gum tissue helps protect the implant and maintain long-term stability. Immediate placement may be less predictable when:
Gum recession is present
Keratinised tissue is limited
Soft tissue is thin
Periodontal disease is active
A delayed approach may give the tissue time to recover or be treated.
4. Systemic Health Influences Healing
Certain medical factors can slow or complicate healing, such as:
Uncontrolled diabetes
Autoimmune conditions
Smoking or nicotine use
Conditions affecting bone metabolism
Medications that alter bone turnover
These do not always exclude immediate placement, but they require careful assessment.
5. Bite Forces and Occlusion Must Be Considered
Even if the implant can be placed immediately, strong bite forces or grinding (bruxism) may interfere with early stability. In such cases, temporary restorations may not be advisable.
6. Expectations Must Match Biological Reality
Immediate placement does not provide instant functional teeth.
The implant still needs time to integrate before it can support chewing.
Clear expectations help ensure safe planning and predictable outcomes.
Immediate Dental Implants at Lara Smile: Safety, Planning and Patient Support
At Lara Smile, immediate dental implants are assessed with a structured clinical approach. The focus is on patient safety, anatomical suitability, and long-term predictability. This section provides general information only. Treatment decisions are made after a full clinical examination by a qualified dentist.
Comprehensive Diagnostic Process
Each patient is evaluated through:
A detailed clinical examination
Radiographic imaging, often including CBCT
Assessment of bone quality and soft-tissue health
Review of any medical conditions that may affect healing
CBCT imaging helps the team analyse bone structure, nerve pathways, sinus position, and potential risks.
Case-by-Case Evaluation
Immediate placement is considered only when conditions support predictable stability, such as:
Adequate bone density
Intact socket walls
Controlled periodontal health
No active infection
Favourable soft-tissue architecture
If these factors are not present, the team may recommend a staged or delayed approach.
Focus on Soft-Tissue and Bone Health
Planning at Lara Smile pays close attention to:
Preserving soft tissue
Protecting socket walls
Evaluating keratinised tissue
Identifying any need for bone grafting
These steps help create a healthy foundation for long-term implant success.
Use of Digital Planning Tools
Digital tools and 3D imaging support precise implant planning.
They help determine:
Implant angle and trajectory
Available bone volume
Safe distances from nerves and sinuses
The relationship between the implant and future restoration
This approach improves accuracy and supports predictable outcomes.
Monitoring, Follow-Up and Patient Guidance
Post-operative care is essential. Patients attend regular follow-ups to monitor:
Tissue healing
Implant stability
Radiographic signs of integration
Oral hygiene practices
During this period, patients receive guidance on how to protect the implant and support healing.
Respect for Treatment Boundaries
Immediate implants are only considered when they match the clinical needs of the case. Lara Smile does not use a one-size-fits-all approach. Each treatment plan is tailored to the patient’s anatomy, oral health, and long-term stability requirements.
Frequently Asked Questions
Immediate dental implants are placed at the same appointment as a tooth extraction, provided that the surrounding bone, soft tissue, and overall anatomy support adequate primary stability. They follow the same biological healing process as conventional implants.
No. Their suitability depends on factors such as bone density, socket integrity, infection status, gum health, and systemic conditions. Only a full clinical examination and radiographic imaging can determine eligibility.
Healing and osseointegration follow the same biological timeline as delayed implants. Immediate placement does not speed up integration; it only changes the sequence of treatment steps.
In some cases, a non-functional temporary restoration may be considered for aesthetic purposes. This depends on implant stability, bite forces, and soft-tissue conditions. It is not appropriate for every case and does not act as a functional final tooth.
They require detailed planning and strict anatomical requirements. The technique itself is not necessarily “better” or “more complex,” but it demands careful evaluation to ensure that primary stability and soft-tissue health can be maintained.
Active or extensive infection may reduce the predictability of immediate placement. In such cases, clinicians may recommend treating the infection and allowing the site to heal before considering implant placement.
The final restoration is typically placed after osseointegration is confirmed through clinical and radiographic assessment. This timeline is similar whether the implant is placed immediately or after healing.